Glaucoma is a disease in which the optic nerve becomes damaged, leading to progressive, irreversible loss of vision. It is often, but not always, associated with increased pressure of the fluid inside the eye.
The nerve damage involves loss of retinal nerve cells typically in a characteristic pattern. There are many different sub-types of glaucoma but they can all be considered a type of optic neuropathy. Raised intraocular pressure is a significant risk factor for developing glaucoma (above 22 mmHg). However one person may develop nerve damage at a relatively low pressure, while another person may have high eye pressure for years and yet never develop nerve damage. Untreated glaucoma leads to permanent damage of the optic nerve and resultant visual field loss, which can progress to blindness. Glaucoma can be roughly divided into two main categories, "open angle" and "closed angle" glaucoma. Closed angle glaucoma usually appears suddenly and is often very painful; visual loss can progress quickly but the discomfort often leads patients to seek medical attention before permanent damage occurs. Open angle, chronic glaucoma tends to progress at a slower rate and the patient may not notice that they have lost vision until the disease has progressed significantly.
Glaucoma has been nicknamed the "sneak robber of sight" because the loss of vision normally occurs gradually over a long period of time and is often only recognised when the disease is quite advanced. Once lost, this damaged visual field cannot be recovered. Worldwide, it is the second leading cause of blindness. Glaucoma affects 1 in 200 people aged fifty and younger, and 1 in 10 over the age of eighty. If the condition is detected early enough it is possible to arrest the development or slow the progression with medical and surgical means.
Diagnosis
Screening for glaucoma is usually performed as part of a standard eye examination. Screening for glaucoma includes the measurements of the intraocular pressure with tonometry. These measurements are compared over each visit in order to monitor possible damage of the optic nerve. Changes in size or shape of the eye, anterior chamber angle examination using gonioscopy, and examination of the optic nerve to look for any visible damage to it, or change in the cup-to-disc ratio and also rim appearance and vascular change are also examined. Optic nerve photographs are also taken as a means of following the glaucoma progression.
A visual field test may also be performed as requested by the Ophthalmologist. The retinal nerve fiber layer can be assessed with imaging techniques such as optical coherence tomography (OCT).Pachymetry to measure central corneal thickness will also be assessed as it can affect the tonometry readings. A thicker-than-average cornea can result in a pressure reading higher than the 'true' pressure, whereas a thinner-than-average cornea can produce a pressure reading lower than the 'true' pressure.
HVF (visual field test)
By the time the central vision is affected, glaucoma can already be so far advanced with almost all peripheral vision permanently lost. The HVF is a test to measure visual fields. It is an automated perimetry, where repeated light stimulus of varying intensities appears in different parts of the field. Fields are graphed on the basis of patient's perception of these lights. Each eye is tested separately; the eye not being tested is covered with a patch. As the patient fixes straight ahead lights of different sizes and brightness flash around the screen, the patient must press the buzzer each time a light is seen. The test is quick and painless.
The results obtained from the patient are then compared with those of the age matched normal population and the amount of damage is quantified. This test is valuable in diagnosing, and monitoring the treatment in patients with glaucoma. Patient being monitored for glaucoma require multiple repeats of this investigation over a period of time to monitor the progression of the disease.
OCT
In glaucoma the nerve fibers are lost, patients with glaucoma are likely to have thinner nerve fiber layer than normal. By measuring changes in nerve fiber layer thickness over time these tests can detect glaucoma progression. The OCT measures the thickness of the nerve fiber layer on the retinal surface just before the fibers pass over the optic nerve margin to form the optic nerve. It then constructs a topographic (3-D) image of the optic nerve, optic cup and measures the retinal nerve fiber thickness. Over time all these can detect loss of optic nerve fibers.
Management
The modern goals of glaucoma management are to avoid glaucomatous damage, nerve damage, preserve visual field and total quality of life for patients with minimal side effects. These requires appropriate diagnostic techniques, follow up examinations and judicious selection of treatments for the individual patient. Although intraocular pressure is only one of the major risk factors for glaucoma, lowering it via various pharmaceuticals, Laser and/or surgical techniques is currently the mainstay of glaucoma treatment.
Medication
Intraocular pressure can be lowered with eye drops. There are several different classes of medications to treat glaucoma with several different medications in each class. As poor compliance with medications and follow-up visits is a major reason for vision loss in glaucoma patients it is essential that patients use the drops as prescribed and follow up with their Ophthalmologists for regular vision checks.
Commonly used medications
- Xalatan, Lumigan and Travatan increase uveoscleral outflow of aqueous humor.
- Timolol, Betagan and betaxolol decrease aqueous humor production by the ciliary body.
- Alphagan works by a dual mechanism, decreasing aqueous production and increasing trabecular outflow.
- Pilocarpine works by contraction of the ciliary muscle, tightening the trabecular meshwork and allowing increased outflow of the aqueous humour.
- Trusopt, Azopt and Diamox lower secretion of aqueous humor by inhibiting carbonic anhydrase in the ciliary body.
Your Ophthalmologist will prescribe one or more of these drops to control your glaucoma. At each review the Ophthalmologist will assess it effectiveness and may change your drops and frequency to suit.
Laser Treatment
Laser trabeculoplasty may be used to treat open angle glaucoma. A laser spot is aimed at the trabecular meshwork to stimulate opening of the mesh to allows more outflow of aqueous fluid. Usually, half of the angle is treated at a time. A new type of laser is now employed that uses a "cold" (non-thermal) laser to stimulate drainage in the trabecular meshwork, this is called SLT.
The SLT uses short pulses of low-energy light to target the melanin, or pigment, in specific cells of the affected eye. In response, the body's natural healing mechanisms go to work to rebuild these cells. The rebuilding process improves drainage and lowers intraocular pressure. Studies show that SLT is an effective way to lowering eye pressure. In addition, SLT may be repeated three to four times.
Laser Treatment for glaucoma
Nd:YAG laser peripheral iridotomy (LPI) may be used in patients susceptible to or affected by angle closure glaucoma. During laser iridotomy, laser energy is used to make a small full-thickness opening in the iris. This opening equalizes the pressure between the front and back of the iris. In people with narrow angles, this can uncover the trabecular meshwork. In some cases of intermittent or short-term angle closure this may lower the eye pressure. Laser iridotomy reduces the risk of developing an attack of acute angle closure.
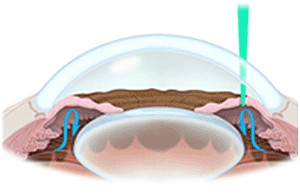
Trabeculectomy The most common conventional surgery performed for glaucoma is the trabeculectomy. Here, a partial thickness flap is made in the scleral wall of the eye, and a window opening made under the flap to remove a portion of the trabecular meshwork. The scleral flap is then sutured loosely back in place. This allows fluid to flow out of the eye through this opening, resulting in lowered intraocular pressure and the formation of a bleb or fluid bubble on the surface of the eye. Scarring can occur around or over the flap opening, causing it to become less effective or lose effectiveness altogether. One person can have multiple surgical procedures of the same or different types.
Glaucoma drainage implants
There are also several different glaucoma drainage implants known more commonly as Molteno implants. These are indicated for glaucoma patients not responding to maximal medical therapy, with previous failed guarded filtering surgery (trabeculectomy). The flow tube is inserted into the anterior chamber of the eye and the plate is implanted underneath the conjunctiva to allow flow of aqueous fluid out of the eye into a chamber called a bleb.